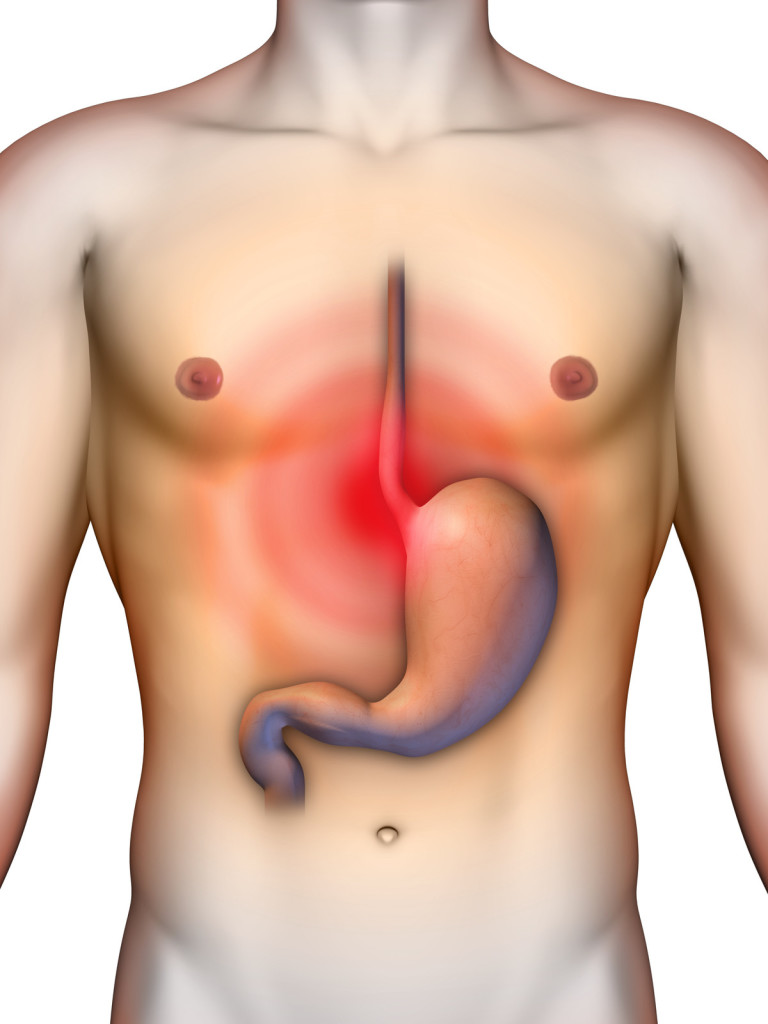
Acid reflux is a common occurance among adults, enough so that outside of the occasional bout of discomfort, we hardly pay it any mind. But for many who suffer from chronic reflux disease, known as GERD, the implications can be much more serious. In particular, GERD is the primary risk factor for esophageal cancer, a fatal disease that usually occurs in the lower part of the esophagus.
Understanding GERD
Acid reflux is when acid backs up from the stomach into the esophagus due to the relaxing of the sphincter muscle that normally keeps digestive juices in the stomach. There are a number of factors that may cause this to become a long-term issue, such as hiatal hernia, obesity, lifestyle factors such as smoking eating habits, and pregnancy.
Gastroesophageal reflux disease (GERD) is very common in our society. Many patients with regular (even one episode per week) heartburn or reflux symptoms treat themselves with over-the-counter antacids. Mostly, these are relatively harmless. However, after a long period of time, acid reflux may lead to a condition known as Barrett’s esophagus, which is a risk factor for esophageal cancer.
Barrett’s esophagus is when the cells lining the walls of the esophagus are modified over time due to chronic reflux. The cell tissue changes until it becomes similar to the structure of the intestine. The reason this is a problem is that it becomes much more likely to develop into cancerous cell tissue over time once this change has taken place.
There are no specific symptoms for those who develop Barrett’s, which is estimated to be about 10% of people who live with chronic GERD. So if you have longterm GERD symptoms (longer than 5 years), it is critical you get screened for esophageal cancer!
Screening for Barrett’s and Esophageal Cancer – The Endoscopy

The process of screening for these diseases is called an upper endoscopy. Once your primary doctor and you have determined the need for this preventive procedure, you’ll need to schedule an appointment with a specialist known as a gastroenterologist. The procedure itself is straightforward and painless. Be sure to have a driver on hand for after the procedure – you’ll be unable to operate a motor vehicle for day!
You are laid on a bed and given sedation medications. Typically, you will be fully unconscious for the procedure, though some doctors may put you in conscious sedation. You should speak with your doctor about this to find out what is right for you. After you are sedated, the gastroenterologist inserts a tube into your mouth and gently advances this tube into your esophagus and deep into the stomach and the small intestine. The endoscopy tube has a light and a camera to visualize your internal gastrointestinal tract. This procedure very accurately examines your entire esophagus for inflammation, ulcers, erosions, bleeding, infections, Barrett’s, and cancer.
If there is evidence or suspicion of inflammation, ulcerations, erosions, Barrett’s, or cancer, biopsies are obtained. Once samples have been taken for biopsy, the procedure will be finished and you’ll be brought back to the waking world. There is typically no lingering pain or discomfort associated with this procedure, though you’ll need to take the rest of the day off and avoid driving or operating heavy machinery due to the drugs remaining in your system.
What your Results Mean
In the event that your gastroenterologist found something he or she didn’t like and took a biopsy, you’ll get the results back, typically within a few days to a week.
- If the initial endoscopy is normal, surveillance EGD may be performed based on future symptoms.
- If Barrett’s esophagitis is diagnosed by biopsy samples (pathologists make a histological diagnosis) but no dysplasia is found (meaning no precancerous cells) you will continue on acid reflux medications, and you will receive a repeat upper endoscopy in three years.
- If Barrett’s is found with low-grade dysplasia, the gastroenterologist will perform an upper endoscopy with extensive biopsy sampling in one year.
- If Barrett’s is found with high-grade dysplasia, but without cancer, doctors take immediate action after discussing options with you.
- If cancer is found, doctors take immediate action after discussing options with you.
When gastroenterologists consider the decision for Barrett’s surveillance, the most critical factors to them are your health, well-being, and survival. This is because esophageal cancer is very fatal.
Your Life with GERD
Patients with established esophagitis or Barrett’s esophagitis typically take a class of medications known as the proton pump inhibitors. The public knows of these medications by their brand names. They are Prilosec, Prevacid, Aciphex, Nexium, Protonix, Zegrid, and Kapidex. Many of these medications are available over the counter without a prescription. The use of proton pump inhibitors may significantly decrease your chances of developing dysplasia, a risk factor of esophageal cancer. They have also been shown to heal erosions and inflammation of the esophagus.
For patients who have no biopsy evidence of Barrett’s esophagitis, medications known as H2 blockers may be used. They includes brand names like Zantac, Pepcid, and Tagamet. Discuss these and other options with your doctor.
Finally, and perhaps most importantly, it is important to manage your diet and lifestyle to keep GERD under control and prevent the onset of esophagul cancer. Smoking, as well as many foods and beverages, such as tomatoes, onions, chocolates, and large volumes of tea, coffee, and carbonated beverages increase acid reflux in many patients. Eating or drinking within 3 hours of lying down can trigger reflux episodes in many patients. And overeating, as well as overindulging in alcohol, tends to trigger reflux in susceptible individuals.
Do your best to learn what triggers your reflux symptoms, and you’ve taken the first step toward better health!