Adult vaccines are just as important as childhood vaccines – the tough part is, you have to remember to get them! Hopefully, this simple chart can help out the next time you schedule a check-up. Remember, it’s on you to keep your doctor up-to-date with your vaccine history!
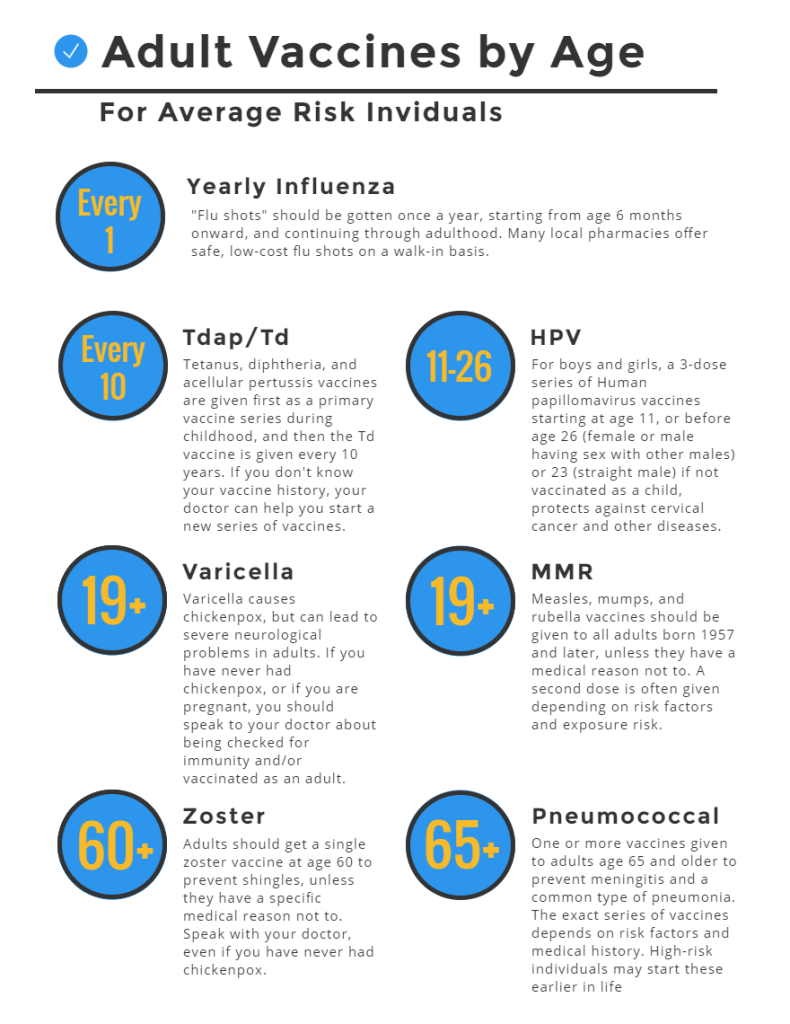
These reminders are for average-risk people only! If you have contraindications, or pre-existing conditions, or are high-risk for certain diseases, you will need to speak to your doctor and will probably be on a very different vaccination schedule. In these cases, it is extremely important that you and your doctor work together to make sure that you are taking the right vaccines at the right times, as your health depends on it.
 The human papilloma virus (commonly known as HPV) is one of the most common sexually transmitted diseases. In fact,
The human papilloma virus (commonly known as HPV) is one of the most common sexually transmitted diseases. In fact,